Summary - Taking NSAIDs increases the risk of you developing stomach ulcers by inhibiting your natural protective system. There are several measures you can take to help get rid of stomach ulcers due to NSAIDs -
1) reduce the dose
2) change the NSAID to one less irritating
3) counteract with other drugs
4) switch from NSAIDs to other pain relievers
4) take Vitamin U
Vitamin U in the form of fresh vegetable juice or supplements can be used in combination with other measures to combat ulcers. However, Vitamin U will not counteract all of these negative effects as NSAIDs are powerful drugs. If you have an ulcer and are taking NSAIDs, talk to your doctor as there may be a solution.
-----------------------------------------------------------------------------------------------------------------------------
Stomach ulcers result from an imbalance between protective and destructive factors. There are several destructive factors including infection with Helicobacter pylori, overproduction of stomach acid, overeating salt, alcohol and sugar, and taking NSAIDs. Ulcers often result from a combination of these factors. The focus of this post is the role NSAIDs play in causing your ulcer.
NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) are widely used to reduce pain and inflammation. The most commonly taken NSAIDs are aspirin (e.g. Bayer), ibuprofen (e.g. Advil, Motrin), naproxen (e.g. Aleve), mefenamic acid (e.g. Ponstal), diclofenac (e.g. Voltaren), piroxicam (e.g. Feldene). A more complete list is linked here.
NSAIDs reduce inflammation and pain by inhibiting the enzyme COX-2. COX-2 is part of your body's inflammatory response. A certain amount of inflammation is good and necessary for healing. However, too much inflammation causes pain and further damage, which is why we take NSAIDs.
How do NSAIDs cause stomach ulcers?
In addition to inhibiting COX-2, NSAIDs also inhibit the related enzyme COX-1, albeit to a lesser extent. COX-1 catalyzes the same reaction as COX-2, that being the synthesis of prostaglandins from arachidonic acid. However, COX-1 and COX-2 have different functions due to their different expression patterns. COX-1 is expressed throughout the body continuously, in contrast to COX-2 which is only expressed during inflammation. In the gastrointestinal tract, the continuous production of prostaglandin E2 catalyzed by COX-1 stimulates mucin production. Mucin forms a mucus bilayer in the stomach that protects the lining against corrosive agents such as stomach acid. The inadvertent inhibition of COX-1 by NSAIDs reduces mucin production, leaving the stomach wall vulnerable. To compound the problem, NSAIDs also have a multitude of other negative effects including increasing the production of stomach acid and increasing oxidative stress (Matsui et al, 2011), which for people with an ulcer will cause more discomfort and make the ulcer worse.
Fortunately, not all NSAIDs inhibit COX-1 equally. Some NSAIDs are more ulcergenic than others. For example, some of the early NSAIDs like aspirin are notorious for upsetting the stomach. More recently, scientists have developed NSAIDs that don't inhibit COX-1 as much as their predecessors and while still inhibiting COX-2 strongly, so-called COX-2 inhibitors, e.g. celecoxib (Celebrex). Consequently, these newer NSAIDs may reduce ulcer formation while still providing pain relief elsewhere in your body. If you have an ulcer and are taking NSAIDs, talk to your doctor about alterative NSAIDs. Be warned that these new generation NSAIDs are not without other side effects.
Can Vitamin U help?
The short answer is probably. Vitamin U is a naturally-occurring nutrient found in all vegetables, fruit and grains. One of its functions is to stimulate the secretion of mucin onto the walls of the stomach. How it does this is not well understood, but it is doesn't seem to have anything to do with COX-1/2 and prostaglandins. As a result, Vitamin U can be used to counteract the mucus-depleting effects of NSAIDs.
Are there any studies supporting the use of Vitamin U to counteract the ulcergenic effects of NSAIDs?
Yes. In 1993, Salim reported the findings of a clinical trial in which Vitamin U was found to accelerate healing of patients hospitalized for erosive gastritis (bleeding from the stomach) caused by NSAID intake. Erosive gastritis is a common precursor to stomach ulcers. The majority of the patients had been taking NSAIDs for either osteo- or rheumatoid arthritis for less than 3 months. The NSAIDs used included diclofenac, piroxicam, mefenamic acid, naproxen and ibuprofen. The double-blind study found that the patients who received 4 x 500 mg of Vitamin U (DL-methylmethionine sulfonium chloride) per day had significantly less bleeding than the negative controls. Similarly to Vitamin U, patients given the sulfhydryl amino acid L-cysteine were also found to have significantly reduced bleeding, demonstrating the action of Vitamin U is likely via its conversion to a sulfhydryl. Endoscopies performed two days after treatment revealed significantly greater healing in those who were given either Vitamin U or cysteine. Of the 57 patients who were not treated with either Vitamin U or cysteine, 4 died from their condition. In contrast, there were no fatalities in those who were treated with either of these compounds.
Currently, it is standard medical practice in cases of erosive gastritis to get the patient to stop taking NSAIDs, or at least take less irritating types, and/or to suppress stomach acid production. For a person who is taking NSAIDs for arthritic pain, reducing the amount of NSAIDs taken is clearly not desirable. Switching to less irritating NSAIDs is an option. Talk to your doctor.
Suppressing acid production will reduce irritation of the stomach, but at what cost? Unless you are producing too much stomach acid (a rare condition), reducing stomach acid will have side effects. The major role of stomach acid is to digest protein in our food. Dietary protein must be unraveled then enzymatically chopped up by pepsin to produce peptides. Without an acidic environment, protein passes through to the duodenum half digested. Enzymes in the duodenum that further digest protein into tiny peptides or amino acids can only do so much, leaving a significant portion of protein to pass into the colon. Consequently, low stomach acid can result in inadequate protein absorption as well as colonic fermentation (smelly gas). Furthermore, long-term suppression of stomach acid production promotes the growth of Helicobacter pylori, a known carcinogen (more).
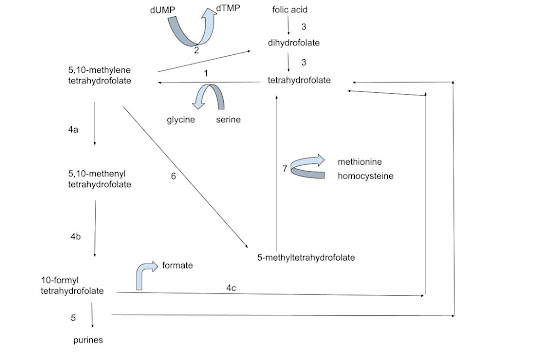
While the results of this clinical trial are promising, Vitamin U is not infinitely powerful. There is only a certain amount Vitamin U can do to reverse or prevent damaged induced by NSAIDs. Large doses of NSAIDs will probably damage the stomach faster than Vitamin U can reverse this damage. However, these findings suggest that Vitamin U may be of some use in counteracting some of the negative effects caused by NSAIDs. Drinking freshly-made vegetable juice on a daily basis provides Vitamin U as well as other beneficial nutrients such as folate.